Engineering The Next Generation Of Lipid Nanoparticles For Advanced Therapeutics
By Life Science Connect Editorial Staff
Lipid nanoparticles (LNPs) have emerged as a transformative technology in drug delivery, driven by the success of mRNA-LNP vaccine formulations in the wake of the COVID-19 pandemic. While their versatility, high transfection efficiency, and relative tailorability have made LNPs a popular gene of interest (GOI) delivery mechanism in the biopharmaceutical development space, challenges linked to their stability in vivo, transience in the bloodstream, and scalability persist.
Recent advances have highlighted that although the composition of LNPs is critical, process parameters like mixing dynamics, buffer compositions, and microenvironmental conditions such as pH and ionic strength are equally vital. These factors influence not only the efficiency of nanoparticle formation but also the physicochemical attributes that determine therapeutic performance.
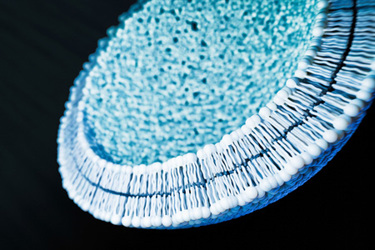
Moreover, the inherent heterogeneity of LNP populations is a focal point of current research: traditional analytical methods like dynamic light scattering (DLS), which offer limited resolution in characterizing particle uniformity, have prompted a shift toward single-particle techniques that can more precisely elucidate the structural and functional variability within LNP batches. At the same time, biological insights are advancing the industry’s understanding of how LNPs behave in vivo — how they interact with cells, avoid immune detection, and deliver payloads with organ- and cell-type specificity.
Ultimately, the convergence of progress in LNP design, process optimization, and biological targeting is paving the way for advancements that will only serve to elevate LNPs as a delivery vehicle for a wider range of molecules and applications.
The Elusive Path to Clinical Translation for LNPs
One of the biggest challenges in the LNP space is also one of the earliest — transitioning bench-scale, preclinical research to clinical development. The hurdles inherent in this translation are rooted in the complex interplay between formulation, manufacturing process, and quality attributes, factors that are still being actively defined and understood in an ever-evolving field. One of the foremost difficulties lies in establishing robust and scalable manufacturing processes that preserve the intended product characteristics. In the chemistry, manufacturing, and controls (CMC) landscape, researchers are often still working to determine which parameters truly matter for LNPs: what to measure, how to measure it, and what those measurements mean in terms of safety, efficacy, and stability.
Unlike more mature modalities such as monoclonal antibodies, LNPs are still undergoing a foundational period of attribute discovery and correlation. Central to this pursuit are the critical quality attributes (CQAs) that serve as the bellwethers for further development. Yet the full picture of which physical and chemical properties of LNPs, such as size distribution, encapsulation efficiency, surface charge, and mRNA-lipid interactions, most impact clinical outcomes — and to what extent — remain elusive for many applications.
Structural characterization of LNPs continues to be particularly challenging. Although ensemble techniques like dynamic light scattering (DLS) are widely used for their convenience, they fail to capture particle heterogeneity, which is now recognized as a key variable in LNP performance. Newer, single-particle methods are being explored, but are not yet broadly implemented or standardized for regulatory purposes. Further complicating the picture is the fact that optimizing one attribute, such as improving encapsulation efficiency, can inadvertently degrade others, like stability or immunogenicity.
Another emerging focus is the detection and minimization of lipid-related impurities and degradation products, including mRNA-lipid adducts. Techniques like reverse-phase ion-pairing liquid chromatography (RP-IPLC) have shown promise in identifying these species, but the industry is still in the early stages of linking such attributes to biological outcomes like immunogenicity, toxicity, and durability. This gap in mechanistic understanding hampers efforts to define clear specifications for clinical products.
Moreover, preclinical successes in targeting or potency do not always translate into clinical viability. Many innovative formulations may show remarkable results in vitro or in animal models, but face major obstacles in terms of manufacturability, reproducibility, or regulatory acceptance. Bridging this gap requires not only a deepening of foundational scientific understanding but also the development of scalable, compliant manufacturing platforms that can consistently deliver quality across clinical and commercial settings.
Finally, it is important to acknowledge that much of the nuanced process knowledge in this space remains proprietary. Although academic and early-stage research continues to generate valuable insights, many industrial advancements are not publicly disclosed due to competitive interests. This creates a fragmented knowledge ecosystem, where shared foundational science coexists with guarded “secret sauce” manufacturing know-how.
Balancing Innovation with Development Complexity
Addressing the challenges of LNP formulation, characterization, and clinical translation requires innovation on several fronts, creating the potential for added complexities that will, in turn, demand coordination across scientific, technical, and regulatory domains. To address the fundamental chemistry and structure-function relationship unknowns surrounding LNP development, companies are expanding lipid libraries and investing in the rational design of ionizable lipids, which serve as the functional cornerstone of most LNP systems. These lipids dictate key properties such as endosomal escape, pKa tuning, and ultimately biodistribution and tolerability. Yet as researchers delve into lipid-by-lipid analyses, they often discover that minor changes in lipid structure can drastically alter pharmacokinetics or tissue tropism, especially across species. This highlights the need for early alignment between biological goals and physicochemical properties.
Parallel to this, new analytical technologies are being adopted to better interrogate LNP structure and behavior at the single-particle level, with the goal of linking CQAs to functional outcomes like transfection efficiency, immunogenicity, or off-target effects. Yet these innovations often create a tension between advancing scientific insight and maintaining regulatory simplicity. For instance, platform regulatory pathways developed during the pandemic can give the impression of uniformity and ease of replication. In reality, even small shifts in formulation composition or process parameters can lead to dramatically different biological performance, especially as LNP applications expand beyond hepatic delivery into more complex tissues and immunologically sensitive contexts.
This expanding toolbox — more diverse lipids, advanced analytics, high-throughput screening, species-specific models — creates both opportunities and challenges. Each new lever introduced into LNP development increases the degrees of freedom in formulation design as well as the potential for unforeseen interactions or development setbacks. In this environment, success demands synergy across teams, disciplines, and stakeholders as opposed to isolated innovation. It requires researchers to not only optimize the lipid or the formulation or the process individually but also co-optimize them in ways that consider downstream effects on manufacturability, safety, and efficacy.
A particularly pressing and underappreciated aspect of LNP development is the need to “choose the winners” earlier in the pipeline by selecting formulations with both in vitro or in small animal model efficacy and a viable path through development and into the clinic. This means moving beyond conventional stepwise screening (mice, then rats, then primates) to more intelligent model selection based on biological relevance, especially when phenomena like the protein corona or organ-specific circulation dynamics can radically alter LNP behavior in larger species. In many cases, failing late in development is not due to poor science but, rather, poor strategy like testing the wrong candidate in the wrong context.
Conclusion
The diversity of LNP applications, whether aiming for immune activation in vaccines or immune silencing in rare disease therapies, means that a “one-size-fits-all” approach is unlikely to be achieved in the near term. Ionizable lipids, for example, must be carefully matched with their cargo and biological targets to achieve consistent performance across animal models and human systems. Even subtle compositional changes can drastically alter biodistribution and therapeutic outcomes, reinforcing the need for intentional design early in development.
From a CMC standpoint, the shift toward smaller, more personalized therapeutic paradigms introduces major hurdles for platform development and facility design. Unlike the global-scale manufacturing of pandemic vaccines, future applications demand flexible infrastructure capable of accommodating a broad range of modalities, doses, and delivery routes, including non-intravenous administration. Each of these routes introduces unique safety considerations — from endotoxins to particle size distributions to residual impurities — that must be carefully characterized and controlled. Moreover, as device-drug combination products become more common, developers must balance formulation needs with device compatibility and regulatory expectations.
To meet these demands, the field must embrace cross-disciplinary innovation. Tools like AI-driven formulation design, barcoding strategies for organ-specific targeting, and organoid systems for preclinical screening offer powerful, though not yet fully matured, ways to bridge the gap between in vitro insights and in vivo performance. Still, these approaches require cautious interpretation and robust validation. Ensuring synergy between discovery, process development, and clinical translation is no longer optional — it is foundational to the success of next-generation LNP-based therapies. Moving forward, the industry's ability to adapt, integrate new technologies, rethink CMC strategies, and deepen its molecular understanding of LNPs, will ultimately determine how far and how fast we can push the boundaries of RNA medicine.
