Advances In Endometrial-Targeted Drug Delivery In Women's Health
A conversation with Saed Abbasi, Ph.D., research faculty, and Laura Ensign, Ph.D., vice chair for research, Johns Hopkins University.
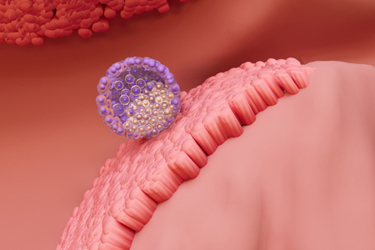
In the U.S., approximately 15% of women have experienced infertility, often with limited understanding of etiology. The endometrium, the inner lining of the uterus, plays a critical role in blastocyst attachment and implantation. Endometrial dysfunction contributes to several women’s health conditions and is associated with implantation failures and poor pregnancy outcomes. Although endometrial targeting has been explored as a therapeutic strategy, it has presented significant challenges.
In this Q&A, Life Science Connect’s Izzy Dininny caught up with Saed Abbasi and Laura Ensign from Johns Hopkins University to discuss the challenges associated with drug delivery in women’s health and how their research has laid the groundwork for future endometrial-targeted therapeutics.
Endometrial dysfunction underlies women’s health conditions ranging from infertility and pregnancy loss to endometriosis and cancer. Why has it been historically underexplored as a therapeutic target despite its clinical relevance?
Abbasi: Early pregnancy is often described as a “black box” because of its complexity and the many coordinated steps required to initiate and maintain a successful pregnancy . Endometrial receptivity remains poorly understood, despite its significant contribution to pregnancy failure and loss. This fundamental gap in understanding of early pregnancy biology continues to hamper the development of effective and targeted therapies aimed at enhancing fertility outcomes.
Ensign: Unfortunately, I think there is still just a gap in funding and attention for areas of women’s health, particularly those related to sexual health and reproduction. There is still a tremendous lack of knowledge about conditions like endometriosis. Further, gender stereotypes have negatively influenced the accuracy of our biological understanding of how fertilization and implantation occur.
Aspects of women’s sexual and reproductive health are often considered taboo, which indirectly diminishes the importance and clinical relevance. Specifically related to infertility, there is also the historical issue of pregnant women being excluded from clinical research, which brings hesitancy to engaging in therapeutic development for issues involving reproduction.
The uterus presents a challenging delivery environment due to cyclic remodeling, mucosal barriers, and systemic clearance. What are the biggest obstacles to achieving precise localized delivery to the endometrium, and how did your team’s approach address them?
Abbasi: Some of the most transformative advances in drug and gene delivery have come from harnessing biological and physiological phenomena that enhance nanoparticle uptake and retention in specific tissues. For example, the gold standard for tumor targeting has long relied on the enhanced permeation and retention (EPR) effect to increase nanoparticle accumulation within tumor microenvironments. Similarly, recent progress in liver-directed genetic medicines has leveraged the liver’s rapid and efficient scavenging of circulating particulates, including therapeutic nanoparticles.
In our recent work, we proposed a new strategy to enhance lipid nanoparticle (LNP) uptake by the endometrium by timing intrauterine infusion to coincide with the window of implantation (WOI). During this phase of the menstrual cycle, the endometrium expresses a rich array of cell-adhesion molecules, such as integrins, which can be targeted with specific ligands to promote nanoparticle binding and cellular uptake.
Ensign: Indeed, our bodies have evolved with numerous layers of physical barriers that can preclude therapeutic delivery, because these barriers function to protect us from pathogens and other exogenous substances that can harm us. Our mucosal surfaces produce secretions that lubricate, protect, and clear unwanted material and waste. The endometrium naturally cycles through shedding and regeneration, though that happens on a longer timescale. These barriers help maintain normal function of the uterus, as well as maintain a largely sterile environment. Thus, we must design systems that can not only bypass the barriers that clear foreign materials away but, in order to enhance specificity, utilize the unique endogenous biology of the target tissue.
Here, we engineered LNPs that can both bypass mucus barriers and interact with cell surface proteins on the endometrium that are enhanced during the window of implantation. This not only increased delivery to the endometrium but reduced the amount of exposure in off-target sites, like the liver. Specificity was further enhanced by utilizing direct infusion into the uterus, which is done clinically with a catheter, similar to how embryos are transferred during in vitro fertilization (IVF).
Your work suggests that localized mRNA delivery can outperform recombinant protein while reducing systemic exposure. How does it outperform, and why? What are the roles of arginylglycylaspartic acid (RGD) and lipid nanoparticles in this method’s success?
Abbasi: A major obstacle to local drug delivery in the uterus is the inherently permeable nature of the uterine environment. Its rich blood supply, extensive lymphatic network, and relatively large tight junctions, compared with those in the gastrointestinal or nasal mucosa, can promote rapid systemic absorption of locally administered therapeutics, resulting in unintended systemic exposure. To address this challenge and improve the localization of protein therapeutics, we combined mRNA and lipid nanoparticle (LNP) technologies.
First, mRNA functions as a prodrug, becoming active only after intracellular translation into the encoded protein. Second, through ligand-conjugation strategies, we serendipitously discovered that decorating the LNP surface with a targeting ligand (RGD) not only enhanced protein expression in endometrial cells after local intrauterine infusion but also reduced expression in off-target organs such as the liver and spleen. While the underlying mechanisms remain to be fully elucidated, we hypothesize that this surface modification alters LNP tropism, enhancing delivery efficiency to endometrial cells while simultaneously reducing delivery in off-target organs such as the liver and spleen.
Taken together, using the targeted mRNA-LNP platform achieved more sustained protein expression in the endometrium and significantly reduced plasma exposure compared to recombinant, both of which are factors that can improve the efficacy and safety of a given therapeutic intervention.
How do your learnings shift the way drug developers should think about dosing, safety, and therapeutic development in women’s health indications?
Abbasi: We believe our work can advance the field by providing a new framework for treating endometrial dysfunction and infertility through precision nanomedicine. Although drug development is often hindered by an incomplete understanding of disease pathogenesis, many widely used therapeutics also remain poorly characterized in terms of their mechanisms of action due to an entangled contribution of both local and systemic effects.
We envision that our targeted mRNA-LNP delivery platform could serve as a powerful tool to disentangle local versus systemic mechanisms of protein therapeutics. By enabling spatially and temporally controlled expression of encoded proteins, this approach has the potential not only to improve safety and efficacy but also to deepen our mechanistic understanding of how these therapies work in the endometrium versus the whole body and during the WOI versus other phases of the menstrual cycle.
Looking ahead, what factors will determine whether endometrium-targeted drugs/therapies can move from investigational status to approved drug product?
Abbasi: This research represents the first demonstration of endometrium-targeted LNP, and the first use of mRNA-based therapy aimed at treating female infertility. Although the path toward clinical translation is promising, significant work is needed before clinical trials. Safety and efficacy must be evaluated in larger animal models, such as nonhuman primates. In parallel, scalable manufacturing processes will need to be established. Dose-escalation studies also will be required, along with careful consideration of clinical variables that influence intrauterine drug administration in humans, such as infusion volume, leakage, and tissue distribution.
Ensign: The most significant factor will be financial. Luckily, prior experience with the COVID-19 vaccines has led to a tremendous expansion of companies and resources available for development of LNP-based products. However, there is a “valley of death” between preclinical validation and reaching clinical trials due to an overall lack of financial resources available to do the kind of GLP and GMP studies that need to be done prior to clinical studies. There are not many grant funding mechanisms and very few foundations that fund these types of IND-enabling studies, and investors are often looking for technologies to be more advanced before investing. That being said, where there is a tremendous unmet need and a well-designed, scalable product like the LNPs we developed, there is a way!
About The Authors:
Saed Abbasi, Ph.D.
 Saed Abbasi, Ph.D., is a research faculty member at the Johns Hopkins University School of Medicine. His work focuses on drug delivery technologies for enabling targeted therapeutics and correcting genetic disorders. His previous research pioneered the use of mRNA for brain gene editing, contributed to the development of safer COVID-19 vaccines, and advanced targeted therapies for the liver and endometrium. Before joining Johns Hopkins, he earned his Ph.D. in Pharmaceutical Sciences from Hokkaido University, Japan. He was also a recipient of the prestigious Japan Society for the Promotion of Science (JSPS) postdoctoral fellowship at the Innovation Centre of Nanomedicine in Kawasaki, Japan.
Saed Abbasi, Ph.D., is a research faculty member at the Johns Hopkins University School of Medicine. His work focuses on drug delivery technologies for enabling targeted therapeutics and correcting genetic disorders. His previous research pioneered the use of mRNA for brain gene editing, contributed to the development of safer COVID-19 vaccines, and advanced targeted therapies for the liver and endometrium. Before joining Johns Hopkins, he earned his Ph.D. in Pharmaceutical Sciences from Hokkaido University, Japan. He was also a recipient of the prestigious Japan Society for the Promotion of Science (JSPS) postdoctoral fellowship at the Innovation Centre of Nanomedicine in Kawasaki, Japan.
Laura M. Ensign, Ph.D.
 Laura M. Ensign, Ph.D., is the Marcella E. Woll Professor of Ophthalmology, the director of the Center for Nanomedicine, and the Vice Chair for Research in the Wilmer Eye Institute at the Johns Hopkins University School of Medicine. She has secondary appointments in Chemical and Biomolecular Engineering, Biomedical Engineering, Physiology, Pharmacology and Therapeutics, Gynecology and Obstetrics, Infectious Diseases, and Oncology. Her research focuses on the principle of characterizing biological barriers in health and disease in order to design more efficacious formulations for prophylactic and therapeutic drug delivery and has already led to the translation of pharmaceutical products that improve clinical management of human disease. She is an inventor on numerous patents licensed to pharmaceutical companies, including many protecting FDA-approved therapies, and she has co-founded three start-up companies at various stages of clinical trials.
Laura M. Ensign, Ph.D., is the Marcella E. Woll Professor of Ophthalmology, the director of the Center for Nanomedicine, and the Vice Chair for Research in the Wilmer Eye Institute at the Johns Hopkins University School of Medicine. She has secondary appointments in Chemical and Biomolecular Engineering, Biomedical Engineering, Physiology, Pharmacology and Therapeutics, Gynecology and Obstetrics, Infectious Diseases, and Oncology. Her research focuses on the principle of characterizing biological barriers in health and disease in order to design more efficacious formulations for prophylactic and therapeutic drug delivery and has already led to the translation of pharmaceutical products that improve clinical management of human disease. She is an inventor on numerous patents licensed to pharmaceutical companies, including many protecting FDA-approved therapies, and she has co-founded three start-up companies at various stages of clinical trials.
